Perianal /
Ischiorectal Abscess (Guda Vidhradhi)
What is Perianal abscess ?
- Perianal abscess (also known as an anal / rectal abscess, anorectal / perirectal abscess,or) is an abscess (a large pocket of infection) adjacent to the anus.
- It arises from an infection at one of the anal crypts of Morgagni which leads to inflammation and abscess formation.
- Most cases of perianal abscesses are sporadic, though there are certain situations which elevate the risk for developing the disease, such as diabetes mellitus, Crohn's disease, chronic steroid treatment and others.
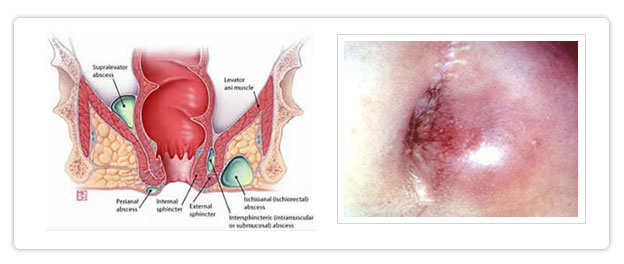
- There are four types of perianal abscesses, anorectal, ischiorectal, intersphincteric, and supralevator.
What are the symptoms of Perianal abscess?
- Pain somewhere around the anal region is the most common symptom of an perianal abscess. The pain may be dull, aching, or throbbing.
- It is worst when the person sits down and right before a bowel movement. After the individual has a bowel movement, the pain usually lessens.
- Other signs and symptoms of perianal abscess include constipation, drainage from the rectum, fever and chills, or a palpable mass near the anus.
- The condition invariably becomes extremely painful, and usually worsens over the course of just a few days.
- The pain may be limited and sporadic at first, but invariably worsens to a constant pain which can become very severe when body position is changed (e.g., when standing up, rolling over, and so forth).
- Depending upon the exact location of the abscess, there can also be excruciating pain during bowel movements, though this is not always the case.
- This condition may occur in isolation, but is frequently indicative of another underlying disorder, such as Crohn's disease.
What causes Perianal abscess ?
- Abscesses are caused by a high density infection of (usually) common bacteria which collect in one place or another for any variety of reasons.
- Anal abscesses, without treatment, are likely to spread and affect other parts of the body, particularly the groin and rectal lumen.
- All abscesses can progress to serious generalized infections requiring lengthy hospitalizations if not treated.
- Historically, many rectal abscesses are caused by bacteria common in the digestive system, such as E. coli. While this still continues often to be the case, there has recently been an uptick in the causative organism being staphylococcus, as well as the difficult to treat community-acquired methicillin-resistant S. aureus.
- Because of the increasing appearance of more exotic bacteria in anal abscesses, microbiological examination will always be performed on the surgical exudate to determine the proper course of any antibiotic treatment.
How is Perianal abscess diagnosed ?
- Diagnosis of perianal abscess begins with a medical history and physical exam.
- Imaging studies which can help determine the diagnosis in cases of a deep non-palpable perirectal abscess include pelvic CT scan, MRI or trans-rectal ultrasound.
- These studies are not necessary, though, in cases which the diagnosis can be made upon physical exam.
How is Perianal abscess treated ?
- Anal abscesses, unfortunately, cannot be treated by a simple course of antibiotics or other medications. Even small abscesses will need the attention of a surgeon immediately.
- Treatment is possible in an emergency room under local anesthesia, but it is highly preferred to be formally admitted to a hospital and to have the surgery (Incision & Drainage and often curettage of the abscess cavity and debridement is necessary) performed in an operating room usually under short general anesthesia.
- If an associated fistula is found then this is usually laid open at the same time. The wound is always left open and packed with gauze and antiseptic solutions.
- Dressings are required for several days. Depending on the size, the wound cavity may take a few weeks to heal.
- The patient does not need to stay in bed and often sent home within twenty-four hours of the surgery, and is instructed to perform several 'sitz baths' per day, whereby a small basin (which usually fits over a toilet) is filled with warm water
mixed with medicated herbal powders and the affected area is soaked for a period of time.
- The patient can fully mobilize and resume normal activities, work etc. while the wound is healing slowly.
- During the week following the surgery, many patients will have some form of antibiotic therapy, along with some form of pain management therapy, consistent with the nature of the abscess.
What is the commonest complication of Perianal Abscess?
- If left untreated or partially treated, an anal fistula will almost certainly form, connecting the rectum to the skin. This requires more intensive surgery in modern system of medicine / Kshara sutra technique which is a non-surgical and safest minimal invasive procedure well practiced in Ayurveda successfully.
- Furthermore, any untreated abscess may (and most likely will) continue to expand, eventually becoming a serious systemic infection such as gangrene of the perineum and general sepsis.